Introduction
In a‚ÄĆ recent growth that has sparked meaningful debate within the medical community,‚Äć the Isle of‚Äć Man’s medical society has raised alarm over the mandate imposed by Manx Care, the island’s healthcare authority.In a‚ÄĆ statement released to the media, the society highlighted a series of concerns ‚Ā£related ‚Ā§to the approaches and policies being adopted under this mandate, asserting that they could have profound implications for the quality of care provided to patients. As stakeholders ‚Ā§in the healthcare sector‚Äć respond to these ‚Ā£assertions, the tensions surrounding ‚ÄĆgovernance and accountability in the NHS ‚ÄĆframework on the Isle of Man are brought into sharp focus. This article explores the key‚Ā§ issues‚Ā£ raised by ‚Äčthe medical society, the potential impact on healthcare delivery, and the broader implications for the future of medical services on the island.
Medical Society‚ĀĘ Raises Alarm Over Implications of Manx ‚ÄčCare Mandate
The‚Ā§ recent proclamation regarding the Manx Care mandate has prompted widespread concern within the ‚Äćmedical community. Experts are especially worried‚Ā£ about how this policy might affect patient care and the operational dynamics of healthcare providers. Among the highlighted issues ‚Äćare:
- Increased Burdens on Healthcare Staff: ‚ÄćThere are‚Äć fears that healthcare professionals may face additional administrative responsibilities, detracting from their primary ‚ÄĆfocus of patient care.
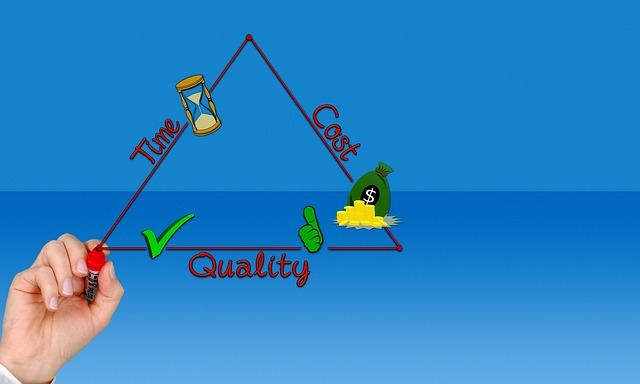
- Potential Compromise of Service Quality: With ‚ĀĘshifts in operational priorities, there is apprehension about the quality of services ‚Ā§delivered to patients, ‚ĀĘespecially‚Äć in critical care areas.
- Impact‚ÄĆ on Recruitment and Retention: The mandate could further complicate efforts to attract ‚Ā§and retain‚Äč essential healthcare workers, leading‚Äć to staffing shortages.
In response to these growing‚ÄĆ concerns, health officials‚ÄĆ have been urged to‚Ā£ reconsider certain ‚ÄĆaspects of the mandate ‚Ā£to ‚Ā£ensure it aligns with the overarching goal of providing optimal patient‚Ā£ care. A recent survey of‚ÄĆ local healthcare providers unveiled a mixed‚Ā§ sentiment regarding the mandate, revealing some additional insights:
| Provider Type | Support for Mandate (%) | Concerns Raised (%) |
|---|---|---|
| General Practitioners | 45% | 80% |
| Nurses | 30% | 85% |
| Specialists | 50% | 75% |
The‚Ā£ stark divide between support and concerns‚Ā£ underscores the imperative‚ÄĆ for open dialog between stakeholders, with the ultimate goal of refining the mandate in ‚Äča way that prioritizes the well-being of both healthcare‚Äč providers and the‚ÄĆ communities they serve.

Concerns About Resource Allocation and‚ÄĆ Staffing Levels Under New Mandate
The medical society has raised‚Äć significant concerns regarding the recent‚Ā£ mandate impacting Manx Care, particularly related to the efficiency of resource allocation and the adequacy ‚ÄĆof staffing levels. Stakeholders fear‚ĀĘ that the new directive may lead to under-resourced facilities, compromising ‚ÄĆpatient‚Äć care. Among the key issues highlighted are:
- Increased Patient Load: ‚ĀĘThe anticipated rise in patient numbers may strain existing ‚ÄĆresources.
- Staffing ‚Ā§Shortages: There are worries that a lack of sufficient trained ‚ÄĆpersonnel could severely affect service delivery.
- Budget ‚ÄĆConstraints: Limited financial resources could impede the ability to hire additional staff or provide necessary training.
Furthermore, the society has called for transparency in ‚ĀĘhow resources are allocated under‚ĀĘ the new mandate. A comprehensive plan detailing staffing ‚ĀĘrequirements and budget distribution ‚Äćis essential to address the current uncertainties.To illustrate the potential challenges faced,the following‚Äć table summarizes the expected vs. actual ‚ĀĘstaffing needs amid the new changes:
| Department | Expected Staffing ‚Ā£Needs | Current Staffing Levels | Shortfall |
|---|---|---|---|
| Emergency ‚Ā£Care | 30 | 22 | 8 |
| Outpatient Services | 25 | 18 | 7 |
| Mental Health Services | 15 | 10 | 5 |

Impact on Patient ‚ÄčCare: medical Society voices Serious Reservations
The recent mandate by Manx Care has sparked significant unease among medical professionals, leading to a ‚Ā£chorus‚ĀĘ of serious reservations voiced‚Äč by the medical society. Practitioners are particularly concerned about the potential implications for patient care quality, safety, and accessibility.they argue that the new directives may inadvertently compromise the well-being ‚Ā£of ‚Ā£patients ‚Äćdue ‚Ā§to ‚Äćincreased bureaucratic hurdles and decreased clinical autonomy. Key points highlighted by practitioners include:
- Patient Safety‚Ā£ Risks: With the stringent guidelines, there is‚ÄĆ anxiety over the possibility of ‚ÄĆdelayed treatments and miscommunications.
- Accessibility Issues: ‚Ā£Some medical society members fear that the changes could ‚Ā§obstruct patients from‚Ā£ receiving timely‚ÄĆ care due to the growing red tape.
- Resource Allocation: Concerns have been raised regarding the redistribution of resources that may detract from ‚ĀĘdirect patient interaction and care quality.
In an effort to clarify ‚Äčand address these concerns, a recent ‚ÄĆmeeting ‚Ā§brought together stakeholders from various sectors of‚ĀĘ the healthcare system. The objectives included ‚Äčcreating a dialogue about‚Ā§ how‚Äć the mandate ‚Ā§could be adapted to‚Äć better serve both‚ÄĆ providers and patients. A preliminary assessment revealed a few areas where amendments could benefit patient care, summarized as follows:
| Area of Concern | Proposed amendment |
|---|---|
| Patient Care Delays | Streamline approval processes‚Äć for urgent cases. |
| Bureaucratic Hurdles | Incorporate feedback mechanisms ‚Äćfor frontline ‚Ā§staff. |
| Communication Gaps | Implement enhanced training programs for staff. |

Addressing‚Ā§ the Concerns: Recommendations for Safeguarding Healthcare Standards
In response to‚ĀĘ the challenges highlighted by ‚Äćthe medical society regarding the‚Ā£ recent Manx ‚ÄćCare mandate, several ‚ĀĘkey recommendations have emerged‚Äč that aim to ‚Ā§reinforce healthcare standards and ensure patient ‚ĀĘsafety.‚ÄĆ Stakeholders emphasize the importance of obvious‚ĀĘ communication among healthcare ‚Äčproviders, policymakers, and the public to foster trust and collaboration. this can be‚Ā£ achieved through regular updates and feedback mechanisms that allow‚ĀĘ for ‚ĀĘcommunity input in healthcare-related‚Ā§ decisions.‚Ā§ Further, providing ongoing education and ‚ĀĘtraining for‚Äć healthcare professionals can definitely help maintain high standards of practice, ensuring that‚Ā§ all staff are‚ÄĆ equipped with the latest ‚Ā§knowledge and skills.
Another crucial aspect of ‚Äčsafeguarding healthcare standards is the implementation of robust monitoring systems to regularly assess the effectiveness of care delivery. Integrating technology, such as data analytics, can‚Äć enable a proactive approach to ‚ĀĘidentifying areas needing improvement.‚ĀĘ Additionally, establishing a framework ‚Ā£for ‚Ā£accountability will encourage adherence to established protocols and best practices, ultimately benefiting patient outcomes. To summarize, the following initiatives are recommended:
- Enhance communication networks within healthcare systems.
- Invest ‚Äćin continuous professional ‚Ā£development programs.
- Utilize data‚Äč monitoring tools for‚Äč real-time evaluations.
- Set clear accountability standards and protocols.
The Future of Manx Care: ‚ÄĆNavigating Challenges and Potential Solutions
The landscape of healthcare on the‚ĀĘ Isle of Man‚Äć is poised for significant change as stakeholders grapple‚Ā£ with ‚Ā§the implications of Manx care’s mandate. recent discussions within‚Äč the medical ‚ĀĘcommunity have highlighted key‚ÄĆ concerns regarding the framework and execution of this ‚Ā§mandate.Practitioners ‚Ā§have raised issues about the adequacy of funding, service delivery, ‚ÄĆand the potential impact‚ÄĆ on patient care. Some of the major points include:
- Funding shortfalls: Concerns that the‚Ā£ current budget may not meet the demands of comprehensive care.
- Workforce engagement: A need for better integration and support for healthcare professionals.
- Patient-Centered approaches: Calls for ‚Äća ‚Ā§focus‚ĀĘ on ‚ĀĘpersonalized care rather than a one-size-fits-all model.
To‚Ā§ address these challenges, potential ‚Ā£solutions are emerging, driven by both healthcare‚ÄĆ professionals‚Ā§ and policymakers‚Äč alike. Proposed strategies aim to foster collaboration between various sectors in healthcare, which could lead to a more robust system. one‚Ā§ approach suggests the establishment ‚ÄĆof a Health Advisory Board ‚ĀĘthat ‚ĀĘcould streamline communication and decision-making. Below is a simplified overview of potential initiatives:
| Initiative | Description |
|---|---|
| Increased ‚ĀĘFunding | Boosting financial support to improve services and facilities. |
| Training Programs | Enhancing skills and knowledge of healthcare workers through‚Äć continuous education. |
| Patient Involvement | Engaging patients in decision-making to improve satisfaction and outcomes. |

Engaging Stakeholders: The Importance of Collaborative Dialogue in‚ÄĆ Healthcare‚ĀĘ reform
In the backdrop ‚Ā§of the ‚ÄĆrecent discourse regarding the Manx Care mandate, the medical society ‚ĀĘhas voiced ‚Äća variety ‚ÄĆof concerns that underscore‚ÄĆ the necessity of fostering collaborative dialogue among‚ÄĆ all stakeholders. The healthcare landscape is not simply‚Äć a series‚Äć of isolated entities; rather, it thrives on the interconnectedness of ‚Ā§patients, healthcare professionals, policymakers, and the ‚Ā§community at large. As reform efforts progress,establishing a platform for open communication will ‚Ā§be crucial in addressing the diverse needs and priorities of these groups. This dialogue will serve as a vehicle‚Äč for identifying‚Äč shared goals ‚Ā£and re-evaluating strategies that promote quality care while ensuring accountability and transparency.
Key areas of concern raised by the medical society highlight potential pitfalls within the current‚ÄĆ framework, including:
- Resource Allocation: Ensuring that resources meet the‚ĀĘ demands ‚Äčof a growing patient population.
- Quality of Care: Maintaining ‚ĀĘand enhancing standards while implementing reform measures.
- Patient Safety: Sustaining ‚Ā§a robust mechanism for addressing safety concerns amidst‚Ā§ changes.
- professional input: Involving healthcare professionals in decision-making ‚Äčprocesses to leverage their expertise.
To facilitate effective‚Äč engagement, it is indeed‚ĀĘ essential to establish structured forums where ongoing feedback loops can‚Äć be created, enabling the integration ‚ĀĘof insights from various perspectives. The dialogue should not only ‚ÄĆfocus on the‚Äč immediate challenges but‚ÄĆ also take a broader view of potential innovations and improvements that could‚Äč redefine healthcare ‚ĀĘdelivery in the Isle‚ÄĆ of Man.
Wrapping Up
the recent outline of concerns‚Ā§ by the ‚ÄĆmedical society‚ĀĘ regarding the Manx Care‚Äć mandate‚ÄĆ highlights a critical juncture for healthcare governance in ‚Äčthe ‚ÄĆIsle ‚Ā§of Man. As stakeholders‚Äć navigate the complexities of healthcare delivery, the points raised underscore the necessity for a cohesive dialogue that encompasses the perspectives of ‚Äčmedical professionals, policymakers, and the ‚Äćcommunity at‚ÄĆ large. Ensuring that ‚Äčpatient care remains at the‚Äć forefront of any mandate‚Ā§ will be essential as Manx Care moves forward. The ongoing discussions will be vital in shaping a framework that balances regulatory compliance with the practical realities of delivering ‚Ā£high-quality health services on the island.As the situation‚ĀĘ develops, both ‚Ā£the medical ‚Äćcommunity and the public will be closely watching how these concerns are addressed‚Ā£ in the coming‚ÄĆ months.