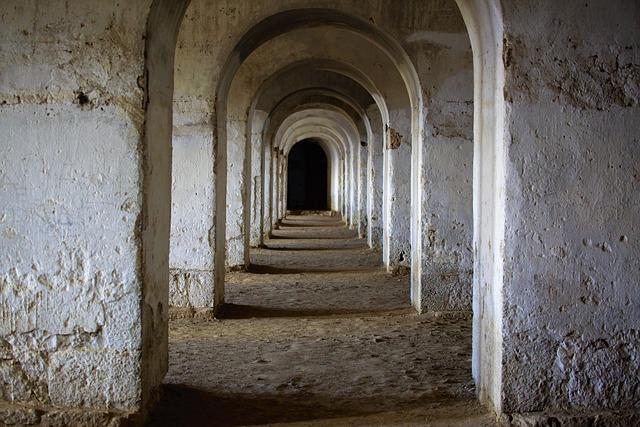
in recent years, the healthcare system in Wales has faced mounting pressures, leading to significant concerns about patient care and safety. A new survey has shed light on a troubling phenomenon known as “corridor care,” where patients are treated in hallways and waiting areas due to overwhelming demand on hospital resources. This practice, which compromises not only the quality of care but also patient dignity, has become alarmingly prevalent across various health facilities in the region. The findings highlight a growing crisis within the Welsh healthcare system, prompting urgent discussions among policymakers, healthcare professionals, and the public. As Wales grapples with the implications of corridor care, understanding its causes and consequences is essential for driving reforms that aim to restore both the integrity and effectiveness of patient care.
Understanding Corridor Care and Its Impact on patient Health
The phenomenon of corridor care, where patients find themselves treated in hallways or other non-designated areas of healthcare facilities, raises significant concerns for patient health outcomes. Factors contributing to this issue include overcrowding, staff shortages, and inefficient resource allocation. As a result, patients may face increased risks of infections, diminished privacy, and delays in treatment, which can lead to worse overall health outcomes. Studies have shown that corridor care can significantly affect the recovery process by creating a disruptive environment that hinders the healing journey.
Moreover, corridor care not only impacts individual patients but also has broader implications for healthcare systems as a whole. Data indicates that increased instances of corridor care correlate with longer hospital stays and higher rates of readmission. The table below illustrates how corridor care can affect key health metrics:
| Health Metric | Impact of Corridor Care |
|---|---|
| Patient Satisfaction | Decreased |
| Infection Rates | Increased |
| Recovery Time | Extended |
| Staff Efficiency | Reduced |
Addressing the causes of corridor care requires innovative solutions, such as improving resource management, investing in staff training, and redefining patient flow protocols. By prioritizing these areas, healthcare systems can mitigate the adverse effects of corridor care, ultimately enhancing patient health outcomes and creating a more effective healthcare environment.

Survey Results reveal the extent of Corridor Care in Welsh Hospitals
The results from the recent survey highlight a troubling trend in Wales’ healthcare system, revealing how corridor care has become prevalent in hospitals across the region. many patients are being treated in overcrowded corridors due to a lack of available beds,which raises serious questions about the adequacy of facilities and staffing levels. The survey documented experiences from both patients and healthcare workers, shedding light on the implications of such an environment on patient safety and care quality. Key findings include:
- Over 70% of respondents reported witnessing patients receiving treatment in corridor settings.
- A significant number of healthcare professionals expressed concerns about the impact on patient dignity and privacy.
- Emergency departments are particularly affected, with waits extending upwards of 12 hours in some cases.
Furthermore, the fallout from the findings has sparked debates among policymakers and healthcare administrators regarding the urgent need for reforms. The growing trend of relying on corridor care underscores the systemic issues that plague Welsh hospitals, including staffing shortages and inadequate infrastructure. To further illustrate the impact of corridor care, the survey revealed the following statistics:
| Patient Concerns | Percentage Affected |
|---|---|
| Delayed treatment | 65% |
| Increased anxiety | 58% |
| Compromised care quality | 72% |

Factors Contributing to the Prevalence of Corridor Care in Wales
the issue of corridor care in Wales is multifaceted, stemming from a combination of systemic and operational challenges within the healthcare system. Resource constraints play a significant role, leading to insufficient staffing levels and a lack of appropriate facilities to accommodate the growing number of patients.Increased patient demand, driven by an aging population and the rise of chronic health conditions, further exacerbates the situation, pushing hospitals beyond their capacity. Additionally, the lack of integrated care between service providers frequently enough results in delays in patient transfers, forcing many individuals to remain in hallways and other non-designated areas for extended periods.
Furthermore, the administrative bottlenecks within National Health Service (NHS) frameworks hinder timely interventions. Issues related to bed blockingŌĆöwhere patients are unable to leave the hospital due to inadequate community care optionsŌĆöalso contribute to hospital overcrowding. This leads to extended wait times for new admissions, perpetuating a cycle where corridor care becomes a temporary solution. To illustrate the impact, consider the following table highlighting key statistical data surrounding patient care experiences:
| Factor | Impact |
|---|---|
| Staffing Shortages | Increased patient load, risk of burnout |
| Aging Population | Higher demand for services, more chronic conditions |
| Administrative Delays | Extended wait times for treatment, inefficient patient flow |
| lack of Integrated care | Fragmented services, longer patient stays |
Strategies for Addressing Corridor Care and Improving patient Flow
The challenge of corridor care necessitates a multifaceted approach that prioritizes patient welfare while streamlining operational efficiencies. Key strategies include the implementation of enhanced triage protocols, which can expedite patient assessments and ensure that those in need receive timely attention. By introducing a centralized patient flow coordinator, hospitals can better manage admissions and discharges, minimizing bottlenecks. This role could be instrumental in facilitating communication between departments, thus reducing wait times and enhancing the overall patient experience.
In addition to refining internal processes, healthcare systems should consider investing in technology solutions that enable real-time tracking of patient locations and status. This can include mobile applications for staff to monitor bed availability and patient flow dynamics.Furthermore, establishing collaborative partnerships with community care providers can ease the pressure on hospitals by ensuring that patients who do not require intensive medical care can access services in a timely manner. focusing on these interconnected areas presents a holistic framework to alleviate the strain of corridor care.

Recommendations for Policy Changes to combat Corridor Care
To effectively address the issue of corridor care in Wales, policymakers must prioritize several strategic changes. First and foremost, there should be an increase in funding for healthcare facilities to ensure they can manage patient inflow and allocate sufficient staff to reduce crowding. Additionally, implementing enhanced training programs would empower healthcare personnel to better handle emergencies and complex cases without resorting to temporary solutions. Key recommendations include:
- Augmenting the workforce: Increase recruitment and retention efforts to bolster staffing levels across critical care areas.
- Expanding community care services: Invest in preventative care and community-based health initiatives to alleviate pressure on hospitals.
- Improving discharge processes: Streamline discharge policies to ensure fast and efficient transitions for patients ready to leave healthcare facilities.
Moreover, integrating technology into the healthcare system can play a pivotal role in alleviating corridor care. By adopting digital solutions such as telehealth services and electronic bed management systems, hospitals can optimize patient flow and reduce wait times. Implementing these innovations may require public-private partnerships to share resources effectively. A potential framework for fostering this collaboration could include:
| Area of Focus | Possible Collaborators | Expected Outcomes |
|---|---|---|
| Technology Integration | private Tech Firms, Local Health Boards | Efficiency in patient management |
| Public Awareness Campaigns | Health Charities, schools | Educated public on available services |
| Community Health Initiatives | Local Governments, NGOs | Improved population health outcomes |

The Role of Healthcare Professionals in Solutions to Corridor Care
The ongoing challenge of corridor care in Wales highlights the critical role that healthcare professionals play in finding effective solutions to this issue. Nurses, doctors, and administrative staff are at the forefront, working tirelessly to ensure that patients receive the care they need even amid resource constraints. Their expertise is essential not only in managing immediate patient needs but also in implementing strategies that can alleviate the pressure on hospital facilities. This includes enhancing communication pathways,optimizing patient flow,and advocating for policy changes that prioritize patient-centered care.
In addition to direct patient care, healthcare professionals are instrumental in educating their peers and the public about the implications of corridor care. Through workshops and community outreach programs, they can effectively convey the importance of seeking timely medical attention and the resources available for support. Moreover, collaboration among healthcare teams can lead to innovative practices that enhance operational efficiency, such as analyzing patient admission patterns and forecasting demands on hospital services. This proactive approach, supported by a commitment to continuous training and adaptation, is vital for mitigating the challenges posed by corridor care.
concluding Remarks
the findings of the recent survey on ‘corridor care’ in Wales paint a troubling picture of the current state of the healthcare system. As patients are left waiting in overcrowded corridors rather than receiving timely treatment, the implications for their health and well-being are profound.Stakeholders at every level must prioritize addressing this endemic issue, implementing effective strategies and reforms to ensure that patient care is restored to its rightful place at the forefront of healthcare delivery. As the ongoing debate continues, it is indeed critical that we hold the relevant authorities accountable and advocate for systems that genuinely put patient needs first. The urgent call to action is clear: Welsh healthcare must adapt to challenges and safeguard the quality of care for all citizens.
















